Resources
How embryo screening can reduce your child’s potential genetic risks
8 min read
Orchid Team

In this guide, we’ll cover what embryo screening for common conditions can potentially do. Along the way, we’ll teach you the basics of the in vitro fertilization (IVF) process. This can help you as you’re considering whether embryo screening is the right option for you.
Orchid Team
What is “embryo screening” and how can it help?
Embryo screening analyzes the DNA of an embryo to flag genetic risks for certain common conditions.
Each embryo has differences in its DNA — siblings only share 50 percent of their DNA with each other, while identical twins have 100 percent the same DNA. Since each embryo has different DNA, each embryo has different genetic risks.
When you conceive at home, chance determines your child’s genetics. When you create embryos through IVF, you can potentially forecast your child’s genetics out of several possible outcomes.
As an example, a couple may have two embryos created through IVF with different risks for coronary artery disease:

*The lifetime risk of coronary artery disease varies based on sex; females on average have a 19.2% chance of developing coronary artery disease by the age of 80, which is lower than for men (Lloyd-Jones, D.M., et al., 2006).
So, in this scenario, you can choose to have a child with a lower risk of heart disease.
If you would like a genetics refresher, review our guide on how to think about genetic risk and what it means.
Besides reporting on genetic risks for common conditions, our embryo test also looks at the amount of genetic material, known as chromosomes, within each embryo. Identifying embryos with the right number of chromosomes increases the chance of IVF success. This is often referred to as preimplantation genetic testing for aneuploidy (PGT-A).
Based on the embryos’ genetic health, patients and their care team can select the embryo with the lowest genetic risk and the best chance of IVF success. Our embryo report prioritizes each embryo according to genetic risk.
The embryo creation and screening process
Here’s how it works:

IVF
Embryos are created through IVF. This involves taking medications to prepare the ovaries for egg collection and fertilizing the eggs with sperm to form embryos.
Embryo Sampling
Five to ten cells are carefully sampled by a trained embryologist from each embryo. DNA from the sampled cells are analyzed to report on each embryo’s genetic risk.

Genetic Report
Receive a genetic risk report for each embryo with guidance from a genetics expert.

Embryo Transfer
Prioritize transfer of embryos with the lowest genetic risk when possible and the best chance of success. The remaining embryos can be frozen for future use.
A step-by-step overview of the IVF process
In vitro fertilization (IVF) involves removing eggs from the ovaries and fertilizing them in the laboratory. With embryo screening, an average IVF cycle takes about 8 to 10 weeks from the beginning of the IVF cycle to embryo transfer. We’ll walk you through the series of key steps and what end outcomes to expect.
9 - 12 days
Ovarian stimulation and egg retrieval
Boost egg production through stimulation medications
During a typical menstrual cycle, only one egg is released. In one round or “cycle” of IVF, the goal is to grow a larger number of follicles, each of which houses an egg, and collect the respective number of eggs.
During this time, the patient will inject themselves with hormone medications at home and visit the IVF clinic to monitor hormone levels through bloodwork and perform ultrasounds to look at follicle growth.
Retrieve eggs from ovaries
The egg retrieval is about a 20-minute procedure under light anesthesia. Once under anesthesia, a fertility doctor will begin the procedure by using ultrasound to guide a small needle, through the vaginal wall, into each ovary to collect the eggs. The eggs are then transferred to the specialized embryology lab.
5 - 7 days
Embryo Transfer
Create embryos by fertilizing eggs with sperm
On the day of egg retrieval, the mature eggs are fertilized with sperm by either surrounding eggs by sperm for one sperm to fertilize the egg or selecting a single sperm to inject directly into the egg. The next day, embryologists check how many mature eggs have fertilized normally.
Grow Embryos
Behind the scenes, embryos grow and develop in an incubator that mimics the environment found in a woman’s fallopian tubes. Many clinics grow embryos until they reach the blastocyst stage, which comprises over a hundred or so cells.
10 - 14 days
Sample embryos for genetic testing and freeze embryos
The embryos that have reached the blastocyst stage by day 5 or 6 are sampled (biopsied) and the sampled cells are sequenced and analyzed.
Embryo screening results take about 10-14 days once the embryo samples are sent. In the meantime, the embryos are frozen and kept safely in the IVF clinic.
Variable
Transfer of embryos into the uterus
Typically frozen embryos are thawed and transferred back to the uterus after the second menstrual period following egg retrieval. This stage depends on the patient's natural menstrual cycle length and when they decide to transfer.
The embryo transfer procedure is not painful and takes a few minutes. The patients are able to watch by ultrasound as embryos are transferred. A follow-up pregnancy test is done about 9 to 11 days after.
How safe is the ovarian stimulation and egg retrieval process? Are there any side effects? Will it hurt?
Some patients may experience bloating, light vaginal spotting and abdominal cramping from the hormone medications similar to a menstrual period. These effects usually subside a few days after egg retrieval. Some women may be at risk of ovarian hyperstimulation syndrome (OHSS). OHSS can be largely avoided and eliminated with close monitoring and medication dosage adjustments. Talk to your fertility doctor to see if you may be at risk.
Recovery from the egg retrieval procedure is brief and patients can return to routine daily activities over the next few days, usually next day. Most patients walk out of the clinic after the procedure about 45 minutes later, taking the rest of the day off to rest.
If I decide to do this, how many transferable embryos will I expect to get from one IVF cycle?
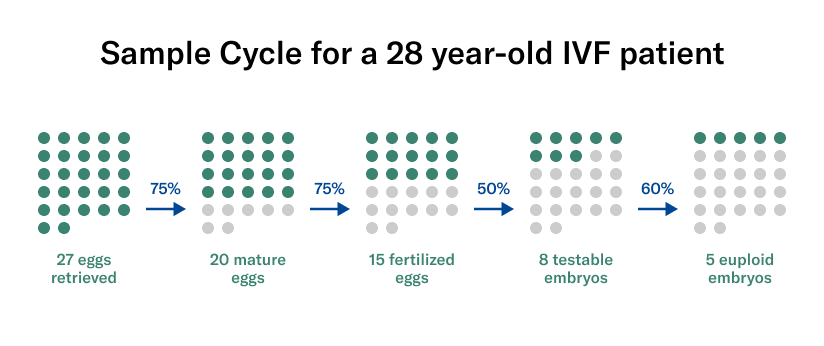
The number of embryos you can get depends on your age, genetics and whether there are underlying causes of infertility. On average, women in their late 20s can expect about 4 to 5 chromosomally normal (euploid) embryos per cycle (Demko et al., 2016). This number decreases with increasing maternal age.
It is typically recommended to transfer only one chromosomally normal embryo at a time (ASRM patient fact sheet, Lee et al., 2016). You can keep any remaining embryos frozen for future use.
Before starting IVF treatment, fertility doctors typically use bloodwork and baseline ultrasounds to get an idea of how many eggs they might anticipate to be able to retrieve. However, it is important to know that eggs and embryos are naturally lost along the way; you do not end up with the same number of embryos as the number of eggs you retrieved.
To illustrate this, we’ve outlined some hypothetical numbers in the embryo creation process for a 28-year-old woman. Remember these are based on averages and can go up or down depending on each individual.
Will this be enough to mitigate genetic risks for a specific condition?
While we cannot guarantee there will be at least one embryo with normal genetic risks for all conditions tested, embryo screening is able to substantially reduce potential risks. This is especially true if your Orchid Couple Report shows that your future child has an increased genetic predisposition to a specific condition.
The genetic makeup of each embryo created during IVF is determined by chance, but we provide you with the most advanced tools available to quantify genetic susceptibility and have the healthiest child possible.
Additional resources about IVF
Orchid offers advanced genetic testing for couples planning on building their family. We use advanced tools and smart, caring humans to help you give your future children the best shot of a healthy life.
Conceive with greater confidence and peace of mind.
2026 Orchid, Inc. All rights reserved.
Terms
Privacy Policy